Medical air mattresses are a cornerstone of modern patient care, primarily serving to prevent and treat pressure ulcers (also known as bedsores or decubitus ulcers). However, not every patient requires this specialized equipment. Identifying the individuals who will benefit most from a medical air mattress is crucial for optimizing patient outcomes, enhancing comfort, and ensuring resources are utilized effectively. This guide will help healthcare professionals and caregivers understand the key indicators and risk factors that necessitate the use of an advanced pressure redistribution mattress.
1. The Critical Problem: Pressure Ulcers
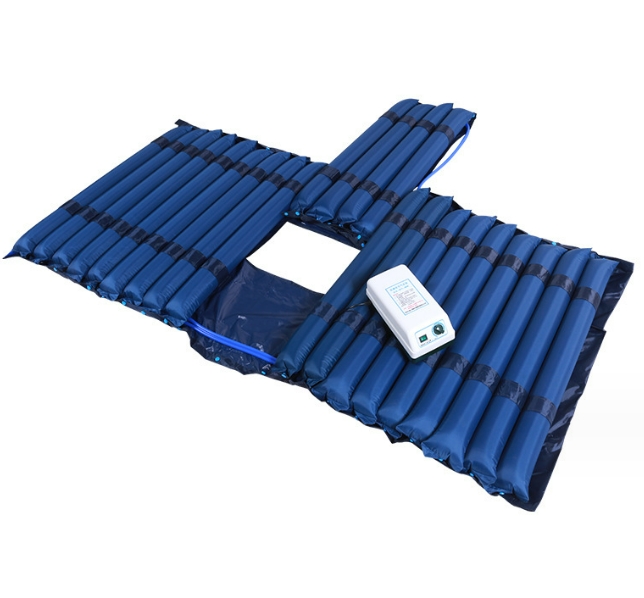
Pressure ulcers are localized injuries to the skin and/or underlying tissue, usually over a bony prominence, resulting from prolonged pressure, or pressure combined with shear and/or friction. They can range from superficial skin discoloration to deep wounds extending to muscle and bone, leading to severe pain, infection, prolonged hospital stays, and increased mortality. Proactive prevention is always the best approach, and medical air cushions are a primary tool in this effort.
2. Key Risk Factors Indicating a Need for a Medical Air Mattress
Patients with one or more of the following risk factors are strong candidates for a medical air mattress:
2.1. Immobility or Severely Limited Mobility
This is the most significant risk factor. Patients who are unable to independently change their position regularly are highly susceptible to pressure ulcers. This includes individuals who are:
- Bedridden: Due to chronic illness, advanced age, or severe injury.
- Paralyzed: From spinal cord injuries, stroke, or neurological disorders.
- Post-Surgical: Especially after extensive surgeries requiring prolonged recovery in bed.
- Sedated or Comatose: Unable to respond to discomfort or reposition themselves.
- Severely Frail or Weak: Lacking the strength to shift their weight.
2.2. Impaired Sensory Perception
Patients who cannot feel pressure, pain, or discomfort are at high risk because they won’t recognize the need to shift their weight. Conditions that impair sensory perception include:
- Neurological disorders (e.g., neuropathy, stroke, spinal cord injury).
- Diabetes with peripheral neuropathy.
- Patients under heavy sedation or anesthesia.
2.3. Nutritional Deficiencies and Poor Overall Health
Adequate nutrition is vital for skin integrity and wound healing. Patients who are:
- Malnourished: Lacking essential proteins, vitamins, and minerals.
- Severely Dehydrated: Affecting skin elasticity and resilience.
- Cachectic (severely emaciated): With very little muscle or fat to cushion bony prominences.
- Suffering from chronic illnesses: Such as cancer, kidney disease, or heart failure, which can compromise circulation and tissue viability.
2.4. Moisture and Incontinence
Excessive moisture on the skin (from perspiration, urine, or feces) can soften the skin (maceration), making it more fragile and susceptible to breakdown, especially when combined with friction or shear. Patients with incontinence or excessive sweating are at increased risk.
2.5. Friction and Shear Forces
Friction occurs when two surfaces rub against each other (e.g., skin against bedsheets). Shear occurs when layers of skin slide in opposite directions over underlying tissue (e.g., when a patient slides down in bed). Both can damage blood vessels and tear tissue, leading to pressure ulcers. Patients who frequently slide down in bed or are difficult to move without dragging are at risk.
2.6. Age
Elderly patients often have thinner, less elastic, and more fragile skin, making them more susceptible to pressure injury. Their slower healing processes also make prevention paramount.
2.7. Underlying Medical Conditions Affecting Circulation
Conditions that compromise blood flow to the skin and tissues increase pressure ulcer risk. These include:
- Diabetes.
- Peripheral vascular disease.
- Anemia.
- Obesity (can lead to pressure in skin folds and difficulty with repositioning).
2.8. Existing Pressure Ulcers
Any patient who already has a pressure ulcer, regardless of its stage, requires an advanced pressure redistribution surface like a medical air mattress to facilitate healing and prevent worsening or new ulcers.
3. The Role of Risk Assessment Tools: The Braden Scale
Healthcare facilities often use standardized tools like the Braden Scale for Predicting Pressure Sore Risk. This scale assesses six key areas: sensory perception, moisture, activity, mobility, nutrition, and friction/shear. A score is generated, and a lower score indicates a higher risk. Patients scoring below a certain threshold (e.g., 18 for adults) are typically identified as being at risk and may require a specialized support surface like a medical air cushion.
4. Beyond Scales: Clinical Judgment and Continuous Observation
While assessment scales are valuable, clinical judgment remains paramount. Healthcare professionals and caregivers should continuously monitor a patient’s skin integrity, especially over bony prominences. Any signs of redness that don’t blanch (turn white) when pressed, tenderness, warmth, or hardness in a localized area could indicate early tissue damage and signal an immediate need for an advanced pressure-relieving surface.
5. Who Should Consider a Medical Air Mattress? A Summary
In summary, consider a medical air Mattress for patients who are:
- Immobile or have very limited mobility.
- Unable to perceive pressure or pain.
- Malnourished or at risk of malnutrition.
- Incontinent or prone to excessive skin moisture.
- Experiencing significant friction or shear.
- Elderly and frail.
- Have underlying conditions compromising circulation or skin health.
- Already have a pressure ulcer.
6. Consulting Healthcare Professionals
It is always recommended to consult with a doctor, a wound care nurse, or a physical therapist. These professionals can conduct a thorough assessment, determine the patient’s specific risk level, and recommend the most appropriate type of medical air Mattress, ensuring optimal patient comfort and therapeutic outcomes.